You now have access to a new era in cardiac imaging with the Cornaris oct imaging system. This technology gives you multimodal imaging tools that let you see and measure artery conditions with unmatched clarity. The Cornaris system merges real-time visualization with automated features, making your workflow faster and safer for patients.
|
Clinical Benefit
|
Impact for You and Your Patients
|
|
Early disease detection
|
Timely interventions and safer procedures
|
|
3D visualization
|
More precise stent placement and better results
|
|
Faster imaging
|
Shorter, safer procedures with fewer complications
|
With this innovation, you can confidently deliver advanced diagnostics and care.
OCT Imaging System Overview
The Cornaris Integrated Multimodal OCT Imaging System brings a new level of precision and efficiency to your Cath Lab. You can use this advanced platform to assess vascular conditions with greater clarity and speed. The system combines multiple imaging technologies, giving you a comprehensive view of the arteries during cardiac procedures.
Multimodal Integration
You benefit from the seamless integration of the oct imaging system with Digital Subtraction Angiography (DSA). This integration allows you to deploy the system immediately in the Cath Lab, saving valuable time during critical procedures. The suspended, compact design keeps your workspace organized and accessible.
Here are the core components and features that support your workflow:
|
Component/Feature
|
Description
|
|
Integration with DSA systems
|
Deep integration with DSA system in Cath Lab for immediate deployment.
|
|
Design
|
Suspended, integrated design saves operating room space.
|
|
Imaging Display
|
Simultaneous display of both OCT and DSA images for the Interventionalist.
|
|
Operational Features
|
Equipped with an OCT foot pedal, tableside controller, and remote-control platform.
|
|
Imaging Capabilities
|
Multimodality imaging features for comprehensive lesion assessment.
|
|
Support for PCI Planning
|
Provides strategic support for PCI planning.
|
With this system, you can view both OCT and angiography images at the same time. This dual display helps you locate lesions quickly and plan stent placement with confidence. The multimodal approach gives you detailed information about vessel walls, plaque, and calcium, all in one session.
Clinical studies, such as the PANOVISION trial, have shown that hybrid imaging systems like this deliver high-quality images without increasing risk. Multimodal integration also enhances plaque characterization, giving you insights that single imaging methods cannot provide.
Real-Time Visualization
You see the benefits of real-time visualization every time you use the oct imaging system. The system provides high-resolution images of vessel walls and lumens, helping you make fast, informed decisions. You can acquire images rapidly, which reduces procedure time and improves patient safety.
-
You can:
-
Instantly visualize vascular structures with both OCT and DSA images.
-
Use the foot pedal and tableside controller to operate the system efficiently.
-
Rely on rapid image acquisition to guide stent placement and assess lesion severity.
The combination of oct and angiography gives you a three-dimensional view of the arteries. This 3D visualization supports accurate diagnosis and treatment planning, especially for complex cases like cerebral aneurysms or severe coronary stenosis.
You use optical coherence tomography to see fine details inside the vessel. The oct imaging system captures images at a resolution of 15 micrometers, allowing you to detect subtle changes in plaque or vessel structure. This level of detail supports early disease detection and precise intervention.
By integrating these advanced imaging tools, you improve your workflow and enhance patient outcomes. The Cornaris system empowers you to deliver safer, more effective cardiac care with every procedure.
System Features

High-Resolution OCT
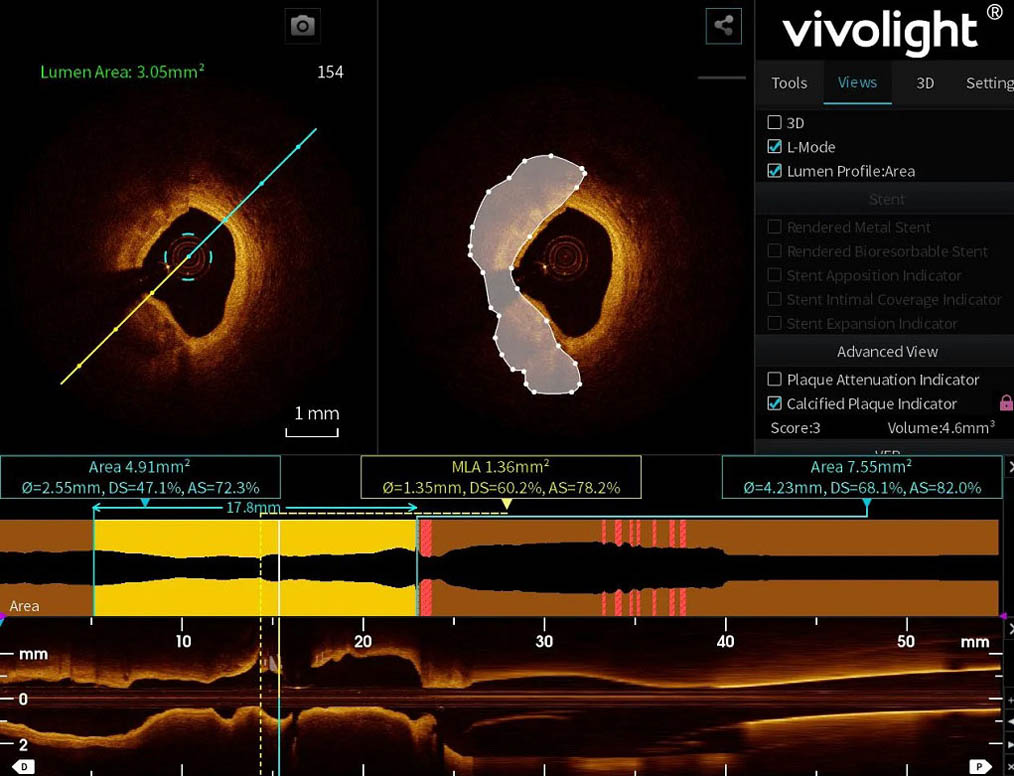
You experience a new standard in vascular imaging with the oct imaging system. The Cornaris platform delivers high-resolution oct images with a precision of 15 micrometers or less. This level of detail allows you to see the smallest features inside blood vessels. You can identify thin-cap fibroatheromas, micro-calcifications, and subtle changes in plaque structure. The oct imaging system captures images at a frame speed of 200 frames per second. This rapid acquisition ensures you do not miss any critical details during a procedure.
When you use oct, you gain a clear advantage in diagnosing and treating complex lesions. The system’s advanced optics and processing algorithms provide exceptional image quality. You can distinguish between different tissue types and assess the severity of blockages with confidence. The clarity of oct images supports early detection of disease and helps you plan interventions with greater accuracy.
Automated Measurements
You save valuable time with the automated measurement features built into the oct imaging system. The system automatically detects the vessel lumen and calculates its dimensions. You no longer need to perform manual tracing or calculations. This automation reduces the risk of human error and ensures consistent results.
The oct platform provides instant measurements of lumen diameter, area, and lesion length. You can review these values on the display as soon as the scan completes. Automated measurements help you quickly assess the need for intervention and monitor the effectiveness of your treatment. You can also use these features to compare pre- and post-procedure vessel conditions.
You rely on these automated tools to streamline your workflow and improve patient safety. The oct imaging system empowers you to focus on clinical decision-making rather than manual data entry.
Workflow Accessories
You operate the oct imaging system with ease using a suite of workflow accessories. The system includes a foot pedal, a tableside controller, and a remote-control platform. These tools allow you to control imaging functions without leaving the sterile field. You can start scans, adjust settings, and review images directly from the tableside.
The foot pedal gives you hands-free operation, which is essential during complex interventions. The tableside controller puts all key functions within your reach. The remote-control platform lets you manage the oct system from outside the procedure room, reducing radiation exposure for you and your team.
Note: Workflow accessories help you maintain focus on the patient and the procedure. You can make adjustments quickly and safely, improving overall efficiency.
You see the impact of these features in your daily practice. The oct imaging system supports a smooth workflow, from patient preparation to image review. You spend less time on equipment management and more time on patient care.
Leading Brands in OCT Imaging Technology
Vivolight is a pioneer in optical coherence tomography (OCT) imaging, driving continuous innovation and setting new standards in cardiovascular diagnostics.
As one of China’s most advanced OCT technology innovators, Vivolight has achieved a compound annual growth rate of over 150% in OCT device sales over the past three years — a testament to its strong clinical adoption and trust from medical professionals.
In 2023, Vivolight became the first Chinese OCT manufacturer to enter global markets, marking a breakthrough in the international development of OCT imaging technology.
Our OCT imaging systems deliver ultra-high resolution, intelligent measurement automation, and seamless workflow integration, empowering clinicians to visualize vascular health with unmatched precision and efficiency.
With cutting-edge optical design and proven clinical performance, Vivolight OCT has become a cornerstone of modern cardiac diagnostics and intervention, helping physicians deliver better care and outcomes for every patient.

Optical Coherence Tomography Technology
You gain a powerful advantage in the Cath Lab with the multimodal features of oct. The Cornaris system lets you evaluate plaque stability, measure stenosis, and assess calcium—all in one session. You do not need extra procedures to get a complete vascular picture.
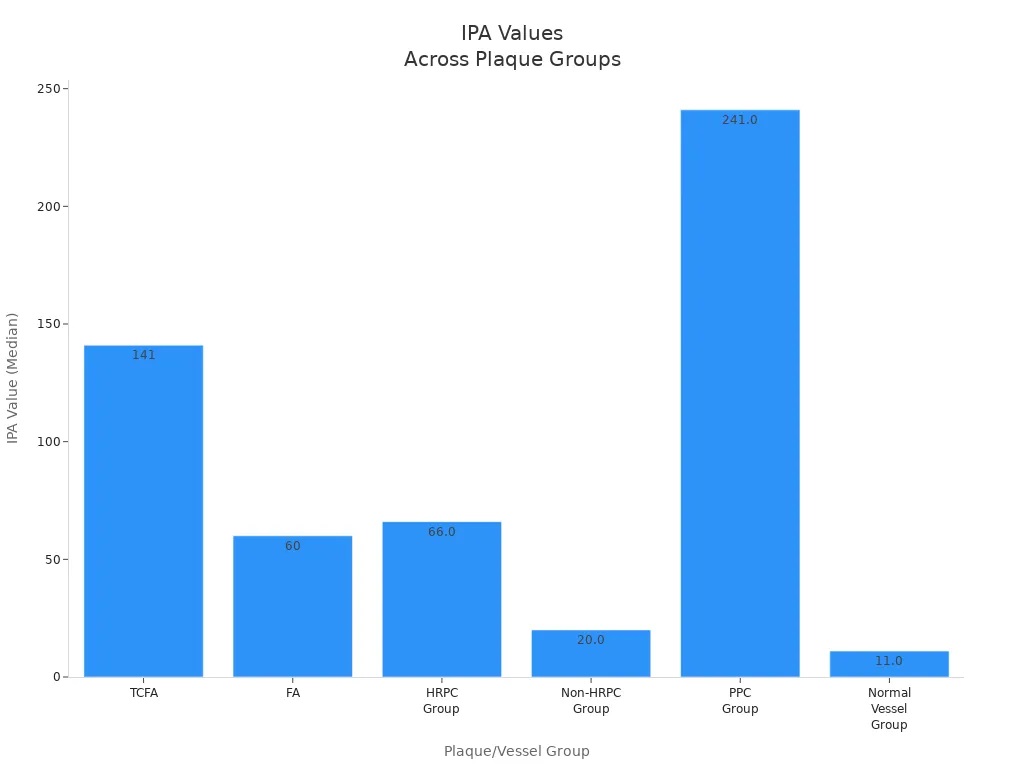
Plaque Attenuation Index
You use the plaque attenuation index (IPA) to assess the stability of arterial plaques. This measurement helps you identify high-risk plaques that may lead to serious events. The oct system calculates IPA values for different types of plaques and vessel conditions. You can see how these values differ in the table below:
|
Finding
|
Value
|
Significance
|
|
TCFA IPA Value
|
141 (98–159)
|
P< .001
|
|
FA IPA Value
|
60 (37–103)
|
P< .001
|
|
HRPC Group IPA Value
|
66.0 (38.0–110.0)
|
P = .001
|
|
Non-HRPC Group IPA Value
|
20.0 (2.0–52.0)
|
P = .001
|
|
PPC Group IPA Value
|
241.0 (155.5–320.5)
|
P < .001
|
|
Normal Vessel Group IPA Value
|
11.0 (3.5–30.5)
|
P < .001
|
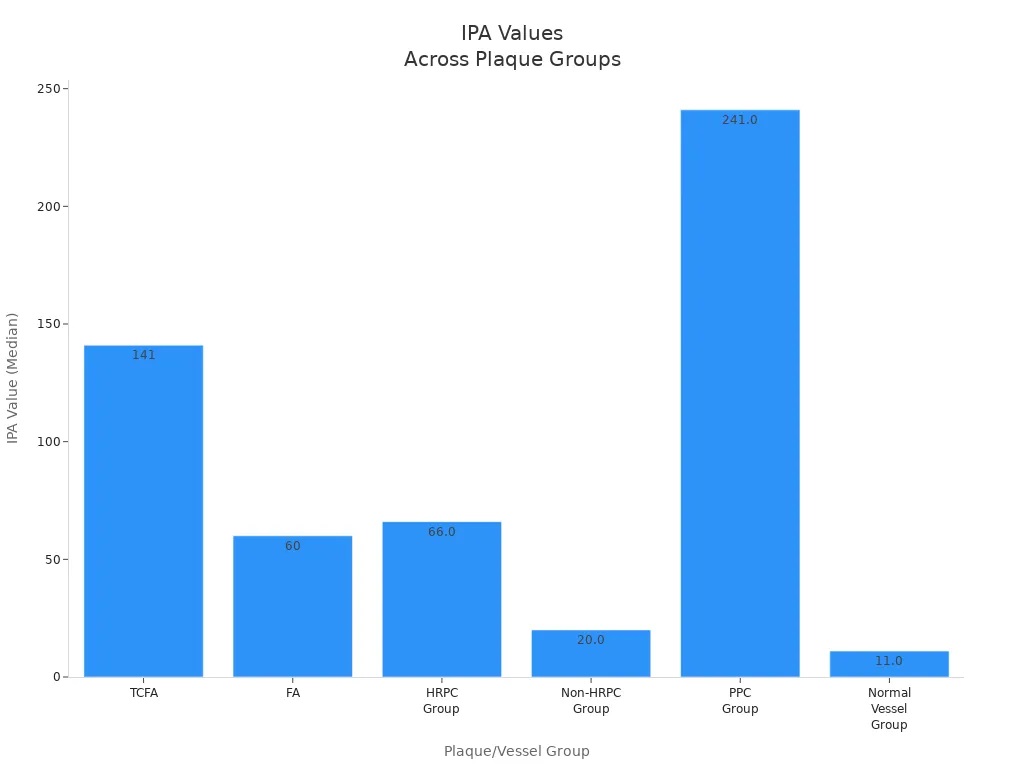
You rely on these numbers to spot unstable plaques early. This approach supports safer and more effective treatment planning.
OCT-Derived FFR
You can use oct to estimate fractional flow reserve (FFR) without extra wires or pressure measurements. This method helps you decide if a lesion restricts blood flow enough to need intervention. Recent clinical trials show that oct-derived FFR matches traditional FFR results very closely:
-
You can use oct metrics to tell positive from negative FFR in intermediate lesions.
-
An oct minimum lumen area (MLA) under 2.0 mm² predicts abnormal FFR with an AUC of 0.80.
-
Combining MLA under 3.1 mm² and area stenosis over 61% gives an AUC of 0.85 for positive FFR in proximal segments.
-
When you combine IVUS and oct, you reach a diagnostic accuracy of 95% for FFR ≤0.80.
-
The area under the curve for this combined method is 0.99, showing excellent predictive power.
You make faster decisions and avoid extra steps by using oct-derived FFR.
Calcium Assessment
You use oct to measure and classify calcium in the arteries. This information guides your treatment plan and helps you avoid complications. The system uses automatic algorithms to detect and quantify calcium. You get details about the location, thickness, and extent of calcium that other imaging methods cannot provide.
-
You benefit from accurate detection and quantification of coronary calcium.
-
You can plan atherectomy or stent placement with more confidence.
-
You reduce the risk of complications and lower costs.
-
High sensitivity for lipid plaque helps you seal dangerous plaques and prevent events.
You complete a comprehensive vascular evaluation with oct in a single procedure. Studies show that this approach adds only a few minutes to your workflow:
|
Study
|
Increase in Procedural Time
|
Additional Notes
|
|
ILUMIEN IV: OPTIMAL PCI trial
|
≈ 18 minutes
|
Multiple OCT runs included
|
|
LightLab Initiative study
|
9 minutes
|
Standardized workflow reduced prep time
|
You save time and improve care by using optical coherence tomography for a full vascular assessment.
Setup and Operation
Initial Setup
You start by preparing the Cornaris system for use in the Cath Lab. Make sure the system is powered on and all connections are secure. Check that the imaging console, display monitors, and workflow accessories are ready. Place the foot pedal and tableside controller within easy reach. Confirm that the Digital Subtraction Angiography system is connected for seamless integration with oct imaging.
Calibration
Proper calibration ensures you get the best image quality from your oct system. Follow these key calibration steps:
|
Calibration Step
|
Description
|
|
k-linearization
|
Corrects for nonlinear wavenumber sampling, essential for optimal resolution.
|
|
Dispersion Compensation
|
Adjusts for dispersion effects in the optical path, improving signal quality.
|
|
Background Removal
|
Subtracts background noise for accurate phase signal retrieval.
|
|
Signal Averaging
|
Reduces random noise, enhancing reliability of calibration results.
|
You should complete these steps before each session to maintain consistent performance.
Patient Positioning
You achieve high-quality oct images by positioning your patient correctly.
-
Ensure patient comfort and stability to reduce motion artifacts.
-
Adjust the chair, tabletop, and chinrest to the right height for adults.
-
For children, use a step stool if needed.
In follow-up visits, register the new images to the baseline scan. This helps you compare measurements accurately and scan the same area each time.
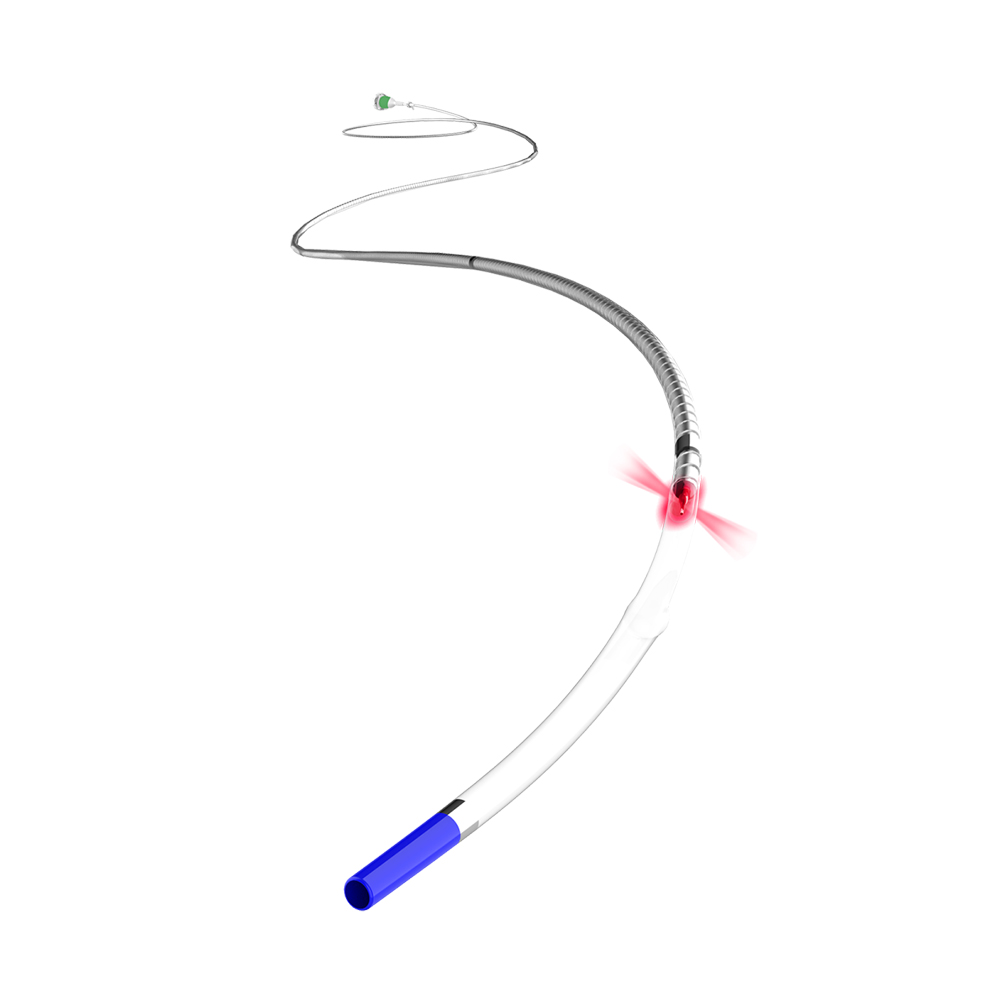
Running OCT Scan
You follow a simple process to run an oct scan:
-
Connect the syringe.
-
Purge the catheter.
-
Drape the DOC.
-
Connect the catheter.
Insert the oct catheter into the vessel. The infrared laser scans the vessel wall in a spiral pattern. The reflected light returns to the device for evaluation, giving you detailed images of the vessel.
Image Fusion
You use the Cornaris system to fuse oct and DSA images in real time. This co-registration lets you see both structural and functional details at once. You can pinpoint lesions, plan interventions, and track outcomes with greater confidence.
Clinical Applications
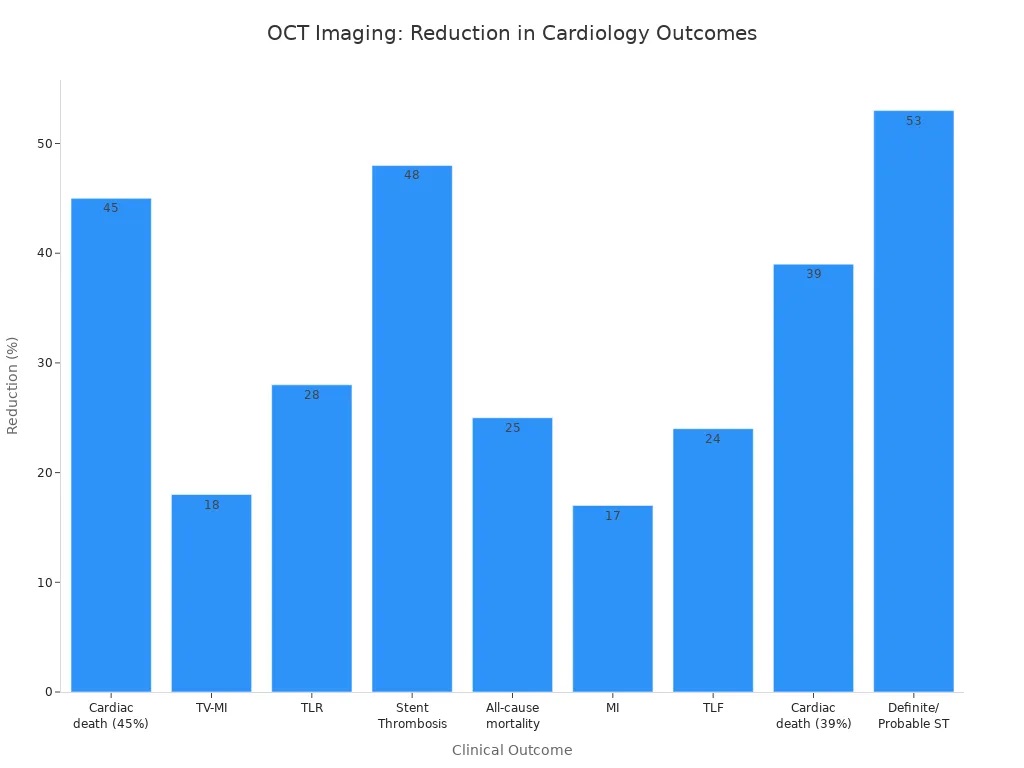
PCI Planning
You use oct to plan percutaneous coronary interventions with greater accuracy. This technology gives you detailed blood vessel imaging, so you can see the structure of the artery and the exact location of lesions. You identify the best spot for stent placement and measure the vessel size with precision. The Cornaris system lets you combine oct with angiography, which helps you make decisions quickly during procedures. You reduce the risk of complications and improve patient outcomes by using this advanced approach.
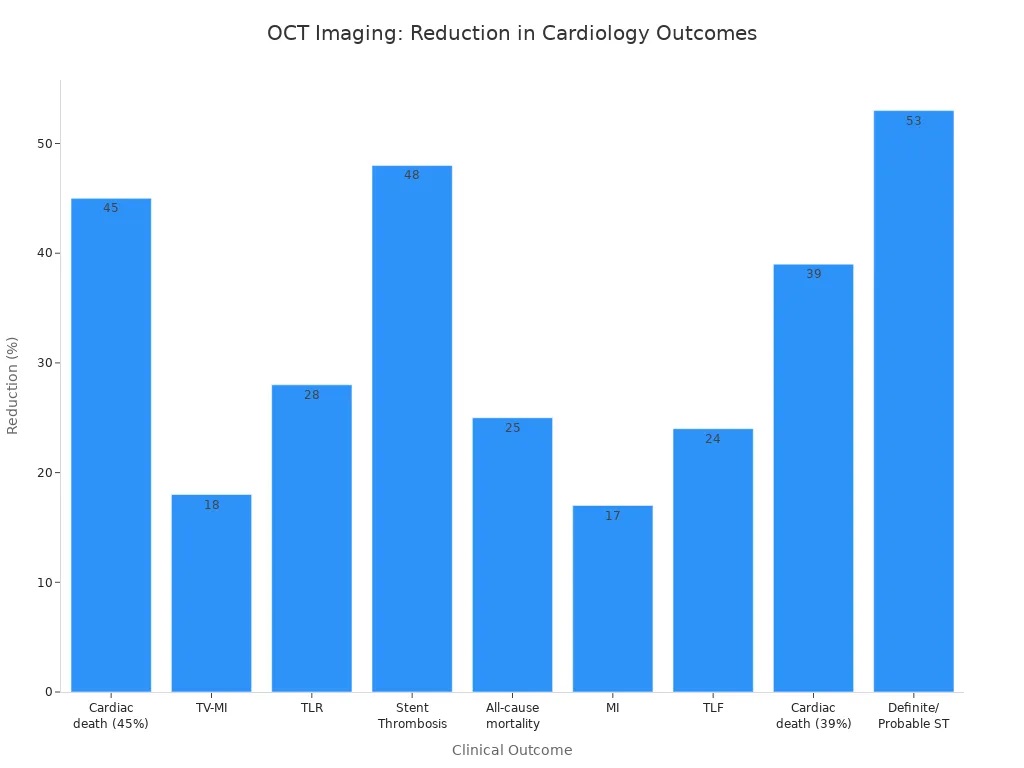
|
Outcome
|
Reduction (%)
|
|
Cardiac death
|
45%
|
|
TV-MI (Target Vessel Myocardial Infarction)
|
18%
|
|
TLR (Target Lesion Revascularization)
|
28%
|
|
Stent Thrombosis (ST)
|
48%
|
|
All-cause mortality
|
25%
|
|
Myocardial Infarction (MI)
|
17%
|
|
Total Lesion Failure (TLF)
|
24%
|
|
Cardiac Death
|
39%
|
|
Definite/Probable Stent Thrombosis
|
53%
|
You see these improvements in real-world cases. Patients experience fewer cardiac events and better long-term results when you use oct-guided PCI.
Workflow Efficiency
You streamline your workflow with the Cornaris system. The tableside controller and foot pedal let you operate the oct system without leaving the sterile field. You save time by using automated measurements and instant image fusion. Non-invasive imaging means you can complete a full assessment in one session. You spend less time switching between devices and more time focusing on patient care. Many clinicians report that oct reduces procedure time and helps them avoid unnecessary steps.
Radiation Reduction
You protect yourself and your patients by reducing radiation exposure. The Cornaris system allows you to control the oct platform remotely, so you can step away from the radiation source during scans. You also need fewer angiographic runs because you get high-quality blood vessel imaging from oct. This approach lowers the total radiation dose for both staff and patients. You create a safer environment in the Cath Lab while maintaining excellent image quality.